The male reproductive system
Male reproductive organs make sperm by the millions. They also transfer those sperm into the female’s reproductive tract, where the sperm can encounter and fertilize eggs. The two jobs involve different subsets of organs and processes.
Organs for Sperm Production
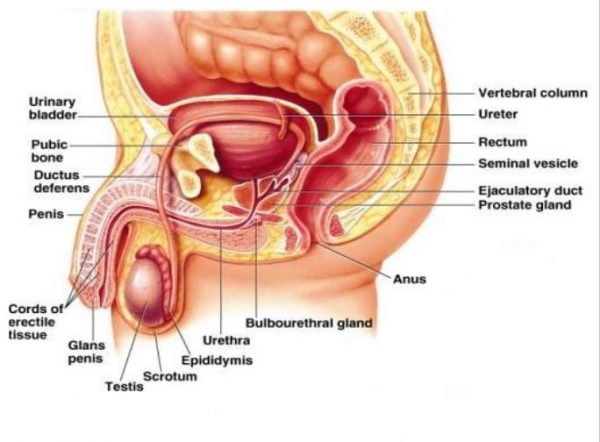
The primary male reproductive organs are the testes (singular, testis) — smooth, oval structures about 4 cm long, held in a bag — scrotum. Each testis is subdivided into about 250 compartments, and each compartment contains several highly coiled, hollow, sperm-bearing tubes called seminiferous tubules, which are 70 cm long. If placed end to end, all the tubules in a man’s testes would make a pipeline several hundred meters long but only about half the thickness of a sheet of paper. Sperm-forming cells (spermatogenic cells) in the tubule walls develop into sperm, while supporting cells in those same walls surround and nourish the developing sperm.
Around the seminiferous tubules lie the interstitial cells (Leydig cells), which produce testosterone and other male hormones.
To develop properly, sperm must have an environment several degrees cooler than the normal internal body temperature. For this reason, the testes hang outside the body in a pouch of skin, the scrotum. If a man wears tight pants, exercises too hard, or sits in a hot tub, the temperature of the scrotum and testes can increase to a point where sperm development temporarily stops. When he cools down, however, the spermatogenic cells can once again develop into sperm.
After attaining their streamlined shape, sperm pass down the cavity of the sperm-bearing tubules and collect in the epididymis, a very narrow tube that is 7 m long and sits coiled tightly on top of the testis. Here, final maturation takes place and the sperm are stored, ready for transport.
Organs for Sperm Transport
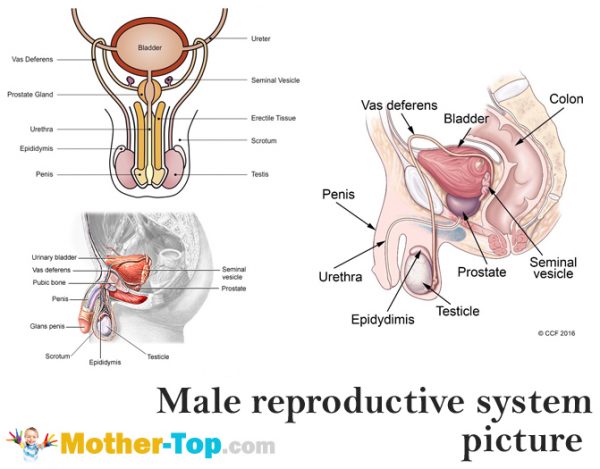
When a male is sexually stimulated during intercourse, masturbation, or even sleep, sperm are rapidly transported and released from the body. The journey begins when smooth muscle cells in the walls of the epididymis contract repeatedly and propel the sperm into the 45 cm long vas deferens, a connecting tube that also has muscular walls that continue to propel the sperm. The vas deferens leads back into the body from the scrotum; near the urinary bladder, it merges with the ejaculatory duct, a duct leading from the seminal vesicle. Secretions from this small gland bathe the sperm in a fluid that contains sugars and other nutrients as well as substances that regulate pH and stimulate muscular contractions in the female reproductive tract.
The combination of sperm and fluid empties into the ejaculatory duct, which passes through the middle of a very important secretory organ, the prostate gland. This chestnut-shaped structure secretes a milky alkaline fluid that mingles with fluid of the seminal vesicle. The added secretion enlarges the volume of sperm and fluid and brings the mixture’s pH to almost neutral. This pH will help neutralize the natural acidity of the female reproductive tract, an acidity that protects her delicate tissues from microorganisms but also tends to inhibit sperm motility.
Once surrounded by milky fluid, the sperm passes from the ejaculatory duct to the urethra. This is a dual-purpose tube that can also carry urine from the bladder out through the penis, a cylindrical organ that transfers sperm to the female. To facilitate entry of the penis into the female’s vagina for intercourse or to clear the urethra, a gland at the base of the penis, the bulbourethral gland, secretes a mucuslike lubricating substance, and spongy erectile tissue within the penis fills with blood and stiffens the entire organ.
At the peak of sexual excitement, ejaculation takes place: Strong muscular contractions of the urethral walls and other muscles forcibly expel semen (sperm plus surrounding seminal fluid, the secretions of the seminal vesicle, prostate gland, and bulbourethral gland) from the penis. While only about 3 milliliters (ml) of semen is ejaculated (a mere teaspoonful), it normally contains 400 million sperm. So many sperm hurtling toward a single egg maximizes the chance for fertilization, and hormones help guarantee a continual supply of viable sperm.
Hormonal Control of Sperm Production
Two types of hormones work together to govern the timing of sperm production. The first hormones are proteins released from two specific parts of the brain. These brain hormones act on cells in the testis, causing one cell type to produce testosterone, a steroid hormone that is related to cholesterol. Testosterone and the other type of brain hormone then act on the testis and stimulate sperm development. Testosterone also travels in the blood back to the brain and blocks further secretion of the brain hormones.
This simple circuit keeps the amount of testosterone— and hence the rate of sperm production—constant. When the testosterone level rises too high, it blocks the release of the brain hormones, and so testosterone is no longer made. But if the testosterone level drops too low, secretion of the brain hormones is not blocked, and they can stimulate the testis to make more testosterone. This kind of regulatory circuit, where a substance like testosterone controls its own concentration, is called a feedback loop. Feedback loops are also important for controlling a woman’s monthly menstrual cycle.




